How do we solve a problem like General Practice?
The King’s Fund (King’s Fund, 2016) describes a crisis in General Practice. Demand, work intensity and the complexity of care continues to increase.
The Problem
Funding and workforce remain overshadowed by substantial workload increases. Face-to-face consultations have increased by 15 per cent and telephone consultations by 63 per cent over 4 years, with GP numbers increasing by 4.75 per cent and practice nurses by 2.85 per cent.
Patients are presenting more frequently, often with multiple co-morbidities, in the context of an aging population and initiatives to move complex hospital care into the community. Population expectations for infallible and timely assessment, diagnosis, treatment and recovery continue to rise, whilst overall satisfaction with service interactions has started to decrease (King’s Fund, 2016).
Unplanned hospital admissions have become a performance measure for the success of General Practice, with access to services a contributor to increasing numbers (Huntley A, 2014). Unplanned admissions are costly, carry morbidity and mortality risks for patients and are disruptive to elective care. Governmental initiatives to increase access to General Practice, may not be the correct strategy and may actually be hindering improvements.
Big data has become the buzzword of the moment, with claims we have now entered the ‘information age’. Advancements in wearable and mobile technology, together with genomics and precision medicine are likely to deluge the modern medical practitioner with patient information. 2020 heralds the year that there will be an estimated 830 million wireless-connected wearables, an increase from 325 million in 2016 (Statista, 2016) .
Various wearable technologies have been developed, and continue to develop, to improve health outcomes (Soh, et al., 2015). As mentioned above, there are challenges currently with managing data. As data is accumulated, guidelines change and patients’ demand more bespoke treatment plans, there presents a significant risk with regards to both safety and litigation.
A glimmer of hope?
A better reduction in unplanned admissions may be achieved through increased continuity of care (Isaac Barker, 2017). More frequent contact with the patient’s regular practitioner can result in 8.96% to 12.49% fewer admissions, depending on whether there was a medium or high level of continuity, respectively (Isaac Barker, 2017).
Continuity of care has also been identified as an important factor for patients (Saultz JW, 2005), correlating with better clinical outcomes (Bankart MJG, 2011; Ionescu-Ittu R, 2007; Freeman GK, 2003) and is often a reason for choosing General Practice as a profession (Kassler WJ, 1991).
The difficult truth
However, fewer GPs have the desire or ability, due to the demands of the job, to work full-time in clinical work. With decreasing numbers of GPs and increasing service utilisation and demand for access, it seems unlikely the demand for continuity is complementary to the demand for access.
The Primary Care workforce is due to decrease further in numbers as tax changes to pensions creates disincentives for older GP partners to work longer. Recruitment problems are also seen with regards GPs, Practice Nurses and Practice Managers (King’s Fund, 2016).
The King’s Fund
There is a clear message from the King’s fund (King’s Fund, 2016) that General practice cannot recover with ‘more of the same’. There is an emphasis to work differently, with new models of care, whilst embracing technological advances.
General Practice cannot recover with more of the same
The King’s Fund 2016
Technology in the NHS
Healthcare often lags behind other areas in its adoption of technology. The reasons are often multifactorial; legacy systems, safety, confidentiality, cost, change and trust play important roles in adopting new technologies. This lag however, provides a unique opportunity to apply technologies from other areas to the area of healthcare.
Repurposing chat bots as an interactive health agent; using neural network algorithms to interrogate data and present conclusions; advances in user interface (UI) technology allowing more intuitive interaction with data, secure communication and information transmission to allow rapid interaction between individuals in Primary Care, Secondary Care and in the community. Direct interaction with appraisal website APIs, allows update of practitioner’s appraisal documentation streamlining much of that process.
Could Electronic Health Records help with continuity?
Technological solutions to the problems in health will likely come in many guises. Digital health spans many areas of many different specialisations, including clinical medicine, computer science, data science, public health, artificial intelligence, wearable technology, robotics and others.
As electronic health records become more detailed, with greater amounts of information, the ability of the healthcare professional to rapidly contextualise the patient becomes more difficult (Singh, et al., 2013; Menon, et al., 2014; Koopman, et al., 2015). Investigations are repeated, there is a loss of ownership of solving the problem and the patient’s experience of the system suffers (Menon, et al., 2014; Koopman, et al., 2015). Continuity of care allows GPs to contextualise the patient without the assistance of the notes. However, could a system that presents information in a more intelligent way, allow a patient to have a ‘continuity experience’ with a health professional they have never met?
Maintaining up to date clinical knowledge in all areas, all of the time, is an impossible task. As humans we have physical limitations of tiredness, emotion, distraction; limitations of information retention and access. An ideal solution would be to take the logical aspects of the General Practioner with its knowledge, data-processing, information-retention and reasoning and place it outside the practitioner.
Allow it to complete activities that require little cognitive ability. Then offer assistance to the practitioner when human clinical knowledge, emotional intelligence, compassionate patient interaction, ethical reasoning, risk analysis and pragmatic decisions about care are required.
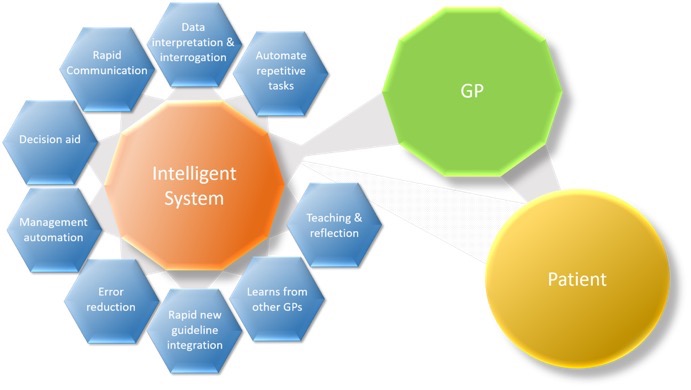
Welcome to a system with “Augmented Intelligence”!
References
- Bankart MJG, B. R. R. A. e. a., 2011. Characteristics of general practices associated with emergency admission rates to hospital: a cross-sectional study. Emerg Med J.
- Freeman GK, O. F. H. P., 2003. Continuity of care: an essential element of modern general practice?. Fam Pract.
- Huntley A, L. D. W. L. e. a., 2014. Which features of primary care affect unscheduled secondary care use? A systematic review.. BMJ.
- Ionescu-Ittu R, M. J. C. A. e. a., 2007. Continuity of primary care and emergency department utilization among elderly people.. CMAJ.
- Isaac Barker, A. S. S. R. D., 2017. Association between continuity of care in general practice and hospital admissions for ambulatory care sensitive conditions: cross sectional study of routinely collected, person level data. BMJ.
- Kassler WJ, W. S. S. R., 1991. Why medical students choose primary care careers.. Acad Med.
- King’s Fund, 2016. Understanding pressures in general practice.. s.l.:s.n.
- Koopman, R. et al., 2015. Physician information needs and the electronic health records (EHRs): Time to reengineer the clinic note. Journal of the American Board of Family Medicine, pp. Vol.28(3), pp.316-323.
- Menon, S. et al., 2014. How context affects electronic health record-based test result follow-up: a mixed-methods evaluation. BMJ Open, p. Vol.4(11).
- Miliard, M., 2017. Epic, Nuance embed AI into EHR for clinical documentation improvement. [Online]
- Saultz JW, L. J., 2005. Interpersonal continuity of care and care outcomes: a critical review.. Ann Fam Med.
- Singh, H. et al., 2013. Information Overload and Missed Test Results in Electronic Health Record-Based Settings. Jama Internal Medicine, pp. Vol.173(8), pp.702-704.
- Soh, P. J., Vandenbosch, G. A., Mercuri, M. & Schreurs, D. M.-P., 2015. Wearable Wireless Health Monitoring: Current Developments, Challenges, and Future Trends. IEEE Microwave Magazine, pp. Vol.16(4), 55-70.
- Statista, 2016. Wearable technology - Statistics & Facts. [Online] Available at: https://www.statista.com/topics/1556/wearable-technology/
Subscribe to digitaldoc
Get the latest posts delivered right to your inbox